Cholesterol is so confusing. In fact, many health experts believe that standard cholesterol tests are outdated and misleading. That is why we recommend and offer the Lipoprotein Particle Profile (LLP) test from Spectracell. It can help you understand if you have the kind lipoproteins (not cholesterol) that can be dangerous. In this blog, written for our partners at Spectrcell Laboratories, you will learn all about the LLP test and how it is different from your standard cholesterol test. This is especially important if you are currently on a statin due to high cholesterol or if you are thinking about getting on a statin. You’ll also get you a full micronutrient chart as it relates to Dyslipidemia (the imbalance of lipids such as cholesterol, low-density lipoprotein cholesterol (LDL-C), triglycerides, and high-density lipoprotein (HDL)), so you can make sure you are sufficient in the micronutrients needed for healthy cholesterol. Becoming micronutrient sufficient and understanding your Lipoprotein Particle Profile can go a long way to helping you achieve extraordinary health, that is why we recommend and offer both the Lipoprotein Particle Profile (LLP) test and the Micronutrient sufficiency test.
Heart disease is still the number one cause of death in America, despite the fact that most Americans are very familiar with cholesterol testing. You commonly hear “I had my cholesterol checked” and it’s normal. Or, “My cholesterol is high so my doctor put me on a statin.” Then, most Americans will (falsely) believe your risk for a heart attack is lowered. Has it ever occurred to you that perhaps the main blood test used for assessing heart disease risk is just, wrong?
Cholesterol tests don’t tell the whole story. In fact, they are grossly misleading. The technology for cholesterol test is decades old and newer, more accurate laboratory testing is available at comparable cost and convenience. Never underestimate the power of momentum, even if that momentum is an outdated, inaccurate, misleading diagnostic test that missed half the people at risk of heart disease for which it is designed to help. The days of cholesterol testing are numbered. As they should be. You deserve a blood test that is more accurate that actually empowers you to lower your heart disease risk. That’s where the LPP® comes in.
What is LPP®?
LPP® stands for Lipoprotein Particle Profile, which is a specialized blood test that assesses risk for heart disease AND what to do about it. It is a replacement for the outdated, and often misleading cholesterol test. LPP® measures the various lipoproteins in your blood, which is important because lipoproteins are what cause heart attacks and strokes, not cholesterol. But not all lipoproteins are equal – some are helpful, and some are incredibly dangerous. The LPP® will tell you which ones you have.
Cholesterol is the “spackle” that fixes arterial damage.
Cholesterol is a substance in our cells that serves several functions – building cell walls, making sex hormones, repairing arteries, for example. The latter of these functions is where cholesterol gets a bad reputation, albeit unfairly. Cholesterol is a sticky substance that is used to “patch” the walls of an artery that has been damaged – sort of like spackling the wall in your house when the sheetrock gets a hole in it. So the real problem is the damage to the artery (the hole in the wall), not the cholesterol (the “spackle”) needed to patch it. Cholesterol is simply the biological “spackle” or “glue” or “paste” or whatever analogy suits you. The cholesterol forms a scab on the inside of the blood vessel. So, often where there is a lot of cholesterol localized in an artery, there is a lot of damage. This can eventually cause blockages (atherosclerosis), or become hard (arteriosclerosis), or form a blood clot (thrombosis).
Lipoproteins cause the trouble, but cholesterol gets blamed.
Lipoproteins are small lipid spheres (think of a hollow rubber ball) that carry cholesterol in the body. Really small lipoproteins act like bee bees to the arterial wall, scratching it and causing damage. Then cholesterol is sent in to patch up this damage. The underlying problem in is the damage to the artery, caused by lipoproteins (and other things like high blood sugar, smoking, inflammation, etc). The vascular damage (the cause) leads to cholesterol build up (the symptom). Cholesterol is not damaging the artery. It is actually trying to repair it.
Proof that cholesterol tests are completely misleading.
Consider this startling statistic: 50% who have a heart attack have normal cholesterol.1,2,3 That means HALF of the cholesterol tests done in medicine will not tell whether or not you are at risk of a heart attack, which is exactly what they allegedly supposed to do. This is why the lipoprotein particle profile test should replace standard cholesterol tests.
Which lipoproteins do you have – healthy or harmful?
LPP® measures your lipoproteins, not your cholesterol, and it tells you the whole range of lipoproteins found in your blood. It is quite comprehensive but in a nutshell, LPP® tells you if you have the dangerous type or healthy type. There are very unique types of lipoproteins that are particularly dangerous, all of which are included in the LPP® panel.
Cholesterol testing isn’t even close.
Then why is cholesterol testing so popular?
The fact that lipoproteins (versus the cholesterol they contain) are what actually cause atherosclerosis has been well established decades ago. But cardiovascular disease (CVD) has been framed a “cholesterol issue” simply because there was no commercial technology for measuring lipoprotein particles until recently. Technology for measuring cholesterol has been widely available for years, so “cholesterol” became synonymous with CVD, when really it is only a surrogate marker. But now that lipoprotein measuring technology is widely available and the cost is comparable to standard cholesterol testing, cholesterol tests are considered very outdated at best, and misleading at worst.
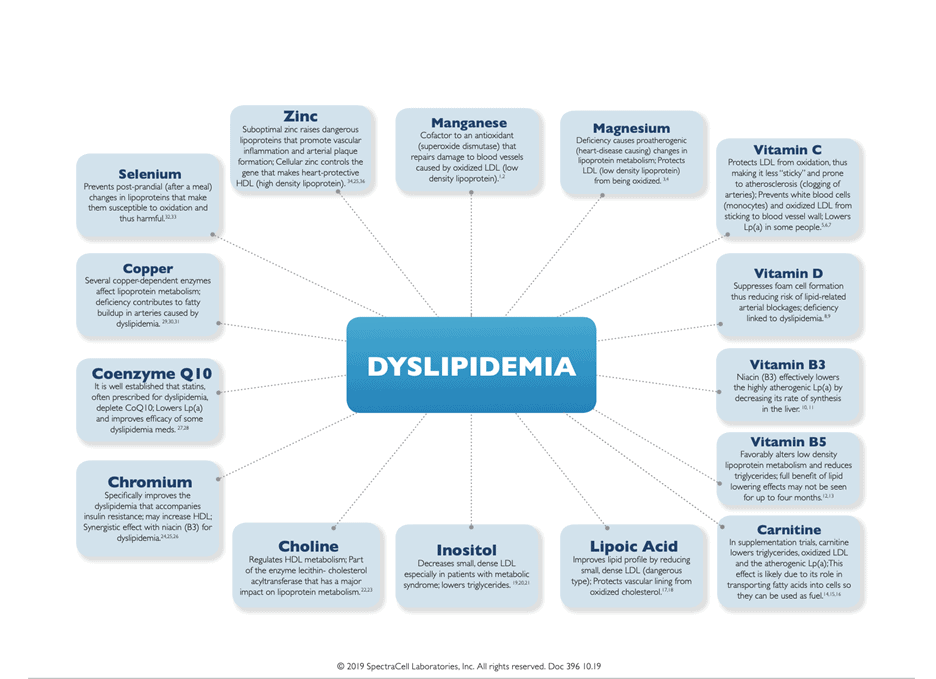
Order your Spectracell LPP® today. But, don’t forget many micronutrients can greatly affect your cholesterol levels. We feel it best to take both the LPP as well as a micronutrient sufficiency test from Spectracell (see here) in order to get the full picture. Just take a minute to view the diagram below. Isn’t it incredible just how many micronutrients may be playing a role in your cholesterol levels (dyslipidemia) if you find yourself deficient.
REFERENCES
Stamler J et al. Is relationship between serum cholesterol and risk of premature death from coronary heart disease continuous and graded? Findings in 356,222 primary screenees of the Multiple Risk Factor Intervention Trial (MRFIT). JAMA 1986;256:2823-2828.
Sachdeva A et al. Lipid levels in patients hospitalized with coronary artery disease: An analysis of 136,905 hospitalizations in Get With The Guidelines. Am Heart J 2009;157:111-117.
Kannel W et al. Efficacy of lipid profiles in prediction of coronary disease. Am Heart J 1992;124:768-774.NIH Publication 05-3290; US Department of Health and Human Services, National Institutes of Health; National Heart, Lung, and Blood Institute; 2005
REFERENCES FOR DIAGRAM
1 Takabe W, Li R, Ai L et al. Oxidized low-density lipoprotein-activated c-Jun NH2-terminal kinase regulates manganese superoxide dismutase ubiquitination: implication for mitochondrial redox status and apoptosis. Arterioscler Thromb Vasc Biol. 2010;30:436-41
2 Perrotta I, Perrotta E, Sesti S et al. MnSOD expression in human atherosclerotic plaques: an immunohistochemical and ultrastructural study. Cardiovasc Pathol 2013;Epub ahead of print.
3 Maier J. Low magnesium and atherosclerosis: an evidence-based link. Mol Aspects Med 2003;24:137-146.
4 Sherer Y, Bitzur R, Cohen H et al. Mechanisms of action of the anti-atherogenic effect of magnesium: lessons from a mouse
model. Magnes Res 2001;14:173-179.
5 Woollard K, Loryman C, Meredith E et al. Effects of oral vitamin C on monocyte: endothelial cell adhesion in healthy subjects.
Biochem Biophys Res Commun 2002;294:1161-1168.
6 Shariat S, Mostafavi S, Khakpour F. Antioxidant effects of vitamins C and e on the low-density lipoprotein oxidation mediated by
myeloperoxidase. Iran Biomed J 2013;17:22-28.
7 Rath M. Lipoprotein-a reduction by ascorbate. J Orthomolec Med 1992;7:81-82.
8 Riek A, Oh J, Bernal-Mizrachi C.Vitamin D regulates macrophage cholesterol metabolism in diabetes. J Steroid Biochem Mol Biol 2010;121:430-433.
9 Guasch A, Bulló M, Rabassa A et al. Plasma vitamin D and parathormone are associated with obesity and atherogenic dyslipidemia: a cross-sectional study. Cardiovasc Diabeto. 2012;11:149.
10 Seed M, O’Connor B, Perombelon N et al.The effect of nicotinic acid and acipimox on lipoprotein(a) concentration and turnover. Atherosclerosis 1993;101:61-68.
11 Kostner K, Gupta S. Niacin: a lipid polypill? Expert Opin Pharmacother 2008;9:2911-20.
12 Rumberger J, Napolitano J, Azmumano I et al. Pantethine, a derivative of vitamin B(5) used as a nutritional supplement, favorably alters low-density lipoprotein cholesterol metabolism in low- to moderate-cardiovascular risk North American subjects: a triple-blinded placebo and diet-controlled investigation. Nutr Res 2011;31:608-615.
13 McRae M.Treatment of hyperlipoprotenemia with pantethine: a review and analysis of efficacy and tolerability. Nutr Res 2005;25:319-333.
14 Malaguarnera M,Vacante M, Avitabile T et al. L-Carnitine supplementation reduces oxidized LDL cholesterol in patients with diabetes. Am J Clin Nutr 2009;89:71-76.
15Sirtori C, Calabresi L, Ferrara S et al. L-carnitine reduces plasma lipoprotein(a) levels in patients with hyper Lp(a). Nutr Metab Cardiovasc Dis 2000;10:247-251.
16 Derosa G, Cicero A, Gaddi A et al.The effect of L-carnitine on plasma lipoprotein(a) levels in hypercholesterolemic patients with type 2 diabetes mellitus. Clin Ther 2003;25:1429-1439.
17 ZhangY, Han P,Wu N et al.Amelioration of Lipid Abnormalities by a-Lipoic acidThrough Antioxidative and Anti-Inflammatory Effects. Obesity 2011;19:1647-1653.
18 Harding S,RideoutT,Jones P. Evidence for using alpha-lipoic acid in reducing lipoprotein and inflammatory related atherosclerotic risk. J Diet Suppl 2012;9:116-127.
19 Maeba R, Hara H, Ishikawa H et al. Myo-inositol treatment increases serum plasmalogens and decreases small dense LDL, particularly in hyperlipidemic subjects with metabolic syndrome. J Nutr Sci Vitaminol 2008;54:196-202.
20 Jariwalla R. Inositol hexaphosphate (IP6) as an anti-neoplastic and lipid-lowering agent. Anticancer Res 1999;19:3699-702.
21 Minozzi M, Nordio M, Pajalich R.The Combined therapy myo-inositol plus D-Chiro-inositol, in a physiological ratio, reduces the cardiovascular risk by improving the lipid profile in PCOS patients. Eur Rev Med Pharmacol Sci 2013;17:537-40.
22 Kunnen S,Van Eck M. Lecithin:cholesterol acyltransferase: old friend or foe in atherosclerosis? J Lipid Res 2012;53:1783-99.
23 Vance D. Role of phosphatidylcholine biosynthesis in the regulation of lipoprotein homeostasis.Curr Opin Lipidol 200819:229-34.
24 Sundaram B, Singhal K, Sandhir R. Anti-atherogenic effect of chromium picolinate in streptozotocin-induced experimental diabetes. J Diabetes 2013;5:43-50.
25 Sealls W, Penque B, Elmendorf J. Evidence that chromium modulates cellular cholesterol homeostasis and ABCA1 functionality impaired by hyperinsulinemia–brief report. Arterioscler Thromb Vasc Biol 2011;31:1139-40.
26 Press R, Geller J, Evans G.The effect of chromium picolinate on serum cholesterol and apolipoprotein fractions in human subjects. West J Med. 1990;152:41-5.
27 Langsjoen P, Langsjoen A.The clinical use of HMG CoA-reductase inhibitors and the associated depletion of coenzyme Q10. A review of animal and human publications. Biofactors. 2003;18:101-11.
28 Cicero A, Derosa G, Miconi A et al. Possible role of ubiquinone in the treatment of massive hypertriglyceridemia resistant to PUFA and fibrates. Biomed Pharmacother 2005 Jul;59:312-7.
29 Hamilton I, Gilmore W, Strain J. Marginal copper deficiency and atherosclerosis. Biol Trace Elem Res 2000;78:179-89.
30 DiSilvestro R, Joseph E, Zhang W et al. A randomized trial of copper supplementation effects on blood copper enzyme
activities and parameters related to cardiovascular health. Metabolism 2012;61:1242-6.
31 Wildman R, Mao S.Tissue-specific alterations in lipoprotein lipase activity in copper-deficient rats. Biol Trace Elem Res
2001;80:221-9.
32 Natella F, Fidale M,Tubaro F et al. Selenium supplementation prevents the increase in atherogenic electronegative LDL (LDL minus) in the postprandial phase. Nutr Metab Cardiovasc Dis 2007;17:649-56
33 Kaur H, Bansal M. Studies on scavenger receptors under experimental hypercholesterolemia: modulation on selenium supplementation. Biol Trace Elem Res 2011;143:310-9.
34 Beattie J, Gordon M, Duthie S et al. Suboptimal dietary zinc intake promotes vascular inflammation and atherogenesis in a mouse model of atherosclerosis. Mol Nutr Food Res 2012;56:1097-1105.
35 Wu J, Wu Y, Reaves S et al. Apolipoprotein A-I gene expression is regulated by cellular zinc status in hep G2 cells. Am J Physiol. 1999;277:C537-44.
36 Shen H, MacDonald R, Bruemmer D et al. Zinc deficiency alters lipid metabolism in LDL receptor deficient mice treated with rosiglitazone. J Nutr 2007;137:2339-45